Why Ultrasonography is Important?
By Dr. Preeti Naware, Consultant Gynecologist & Infertility Specialist
Ultrasonography — often simply called an ultrasound — is one of the most indispensable tools in modern women’s health care. As a gynecologist and obstetrician, I have witnessed firsthand how ultrasound transforms diagnosis, monitoring, and treatment in ways no other modality can.
What Is Ultrasonography?
Ultrasound uses high-frequency sound waves to generate real-time images of internal organs, tissues, and blood flow. It is safe, non-invasive, and does not use ionizing radiation. This makes it highly suited for repeated use, especially in sensitive areas such as the reproductive organs and during pregnancy.
Key Roles in Gynecology & Obstetrics
Pregnancy Monitoring & Fetal Assessment
From the moment pregnancy is confirmed, ultrasonography helps us track embryonic and fetal development. It enables us to:
- Confirm the gestational sac, fetal heartbeat, and viability
- Estimate gestational age and growth parameters
- Monitor amniotic fluid volume and placental position
- Detect multiple pregnancies (twins, triplets)
- Identify potential complications such as fetal anomalies, growth restriction, or placenta previa
Diagnosing Gynecological Conditions
In the non-pregnant state, ultrasound is vital for evaluating a broad range of women’s health issues:
- Uterine fibroids and polyps
- Ovarian cysts, masses, or tumors
- Endometriosis (especially through transvaginal ultrasound)
- Uterine anomalies (e.g. bicornuate uterus, septum)
- Polycystic ovary syndrome (PCOS)
- Pelvic inflammatory disease and adnexal pathology
Guiding Procedures & Treatments
Ultrasound is used during minimally invasive interventions for better accuracy and safety:
- Guided biopsies of pelvic masses
- Follicular monitoring during fertility treatments
- Aspiration of cysts or fluid collections
- Guidance during intrauterine procedures
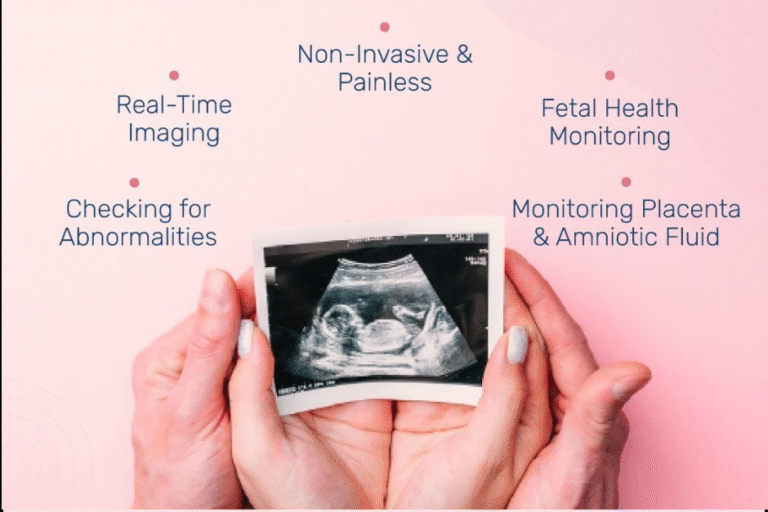
Benefits of Ultrasonography
- Safe for Mother & Fetus — No radiation exposure, making it the modality of choice in pregnancy.
- Real-Time Imaging — Allows dynamic evaluation (movement, blood flow, pulsations).
- Repeatable & Accessible — Can be repeated frequently without harm, and is widely available in most clinics/hospitals.
- Cost-Effective — Less expensive than many imaging modalities (e.g. CT, MRI).
- High Diagnostic Efficiency — Gives clear, detailed imaging of pelvic structures, often obviating the need for more invasive diagnostics.
Limitations & Considerations
- Operator Dependency: The quality and interpretation of ultrasound depend heavily on the skill and experience of the sonographer or clinician.
- Limited Penetration: In obese patients or when bowel gas intervenes, the imaging quality may degrade.
- Resolution Constraints: Very small lesions ( a few millimeters) or deep‐seated structures may not be resolved well.
- False Positives/Negatives: Some findings may be ambiguous and require further evaluation (e.g. MRI or diagnostic laparoscopy).